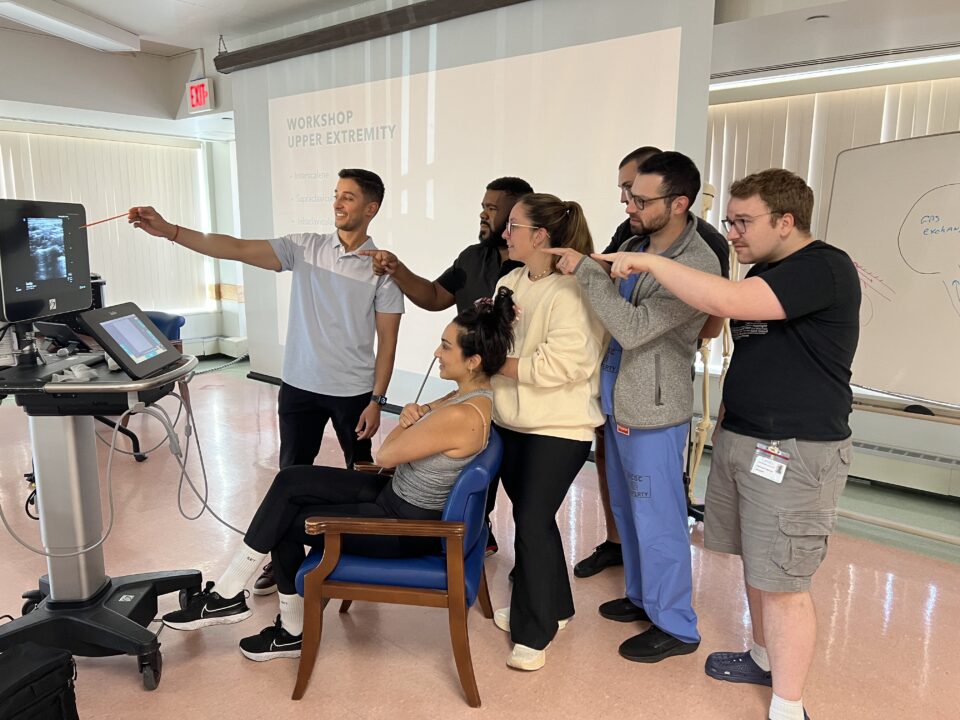
Hurray! We Sono-matched!
November 17, 2021
Last didactic conference in 2021
December 22, 2021A 35 year old male drove himself to the Emergency Department complaining of a stab wound just prior to arrival and told the team “don’t let me die”.
Challenge accepted.
The ED team led by our very own Associate Program Directors, Dr. Max Cooper and Dr. Karima Sajadi-Ernazarova, responded to the trauma Level 1 activation with exceptional Crozer EM residents – Dr. Brian DeBaun, Dr. Raghav Sahni and Dr. Craig Schaaf and the very best nursing staff.
THE PHYSICAL EXAM
Airway: intact
Breathing: bilateral breath sounds but diminished on left with noted stab wound to left lateral chest
Circulation: palpable pulses throughout
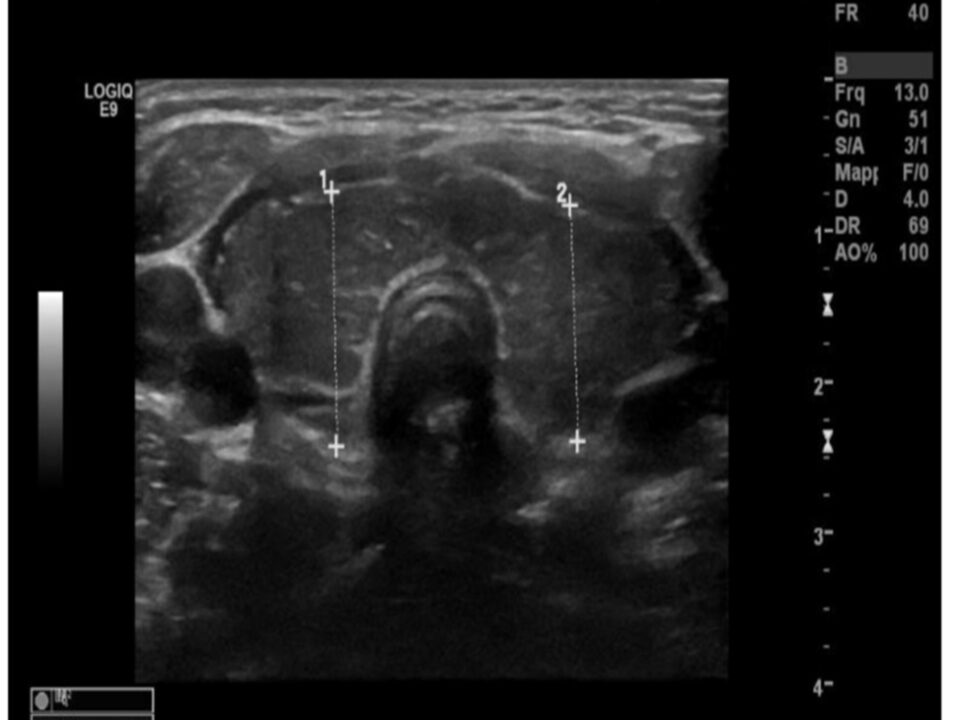
THE ULTRASOUND EXAM:
Dr. Cooper, Crozer Ultrasound Director, placed a phased array probe on the chest and obtained a parasternal long axis view which demonstrated right ventricular diastolic collapse with moderate pericardial effusion. Moments later, the patient developed hypotension and described worsening dyspnea.
THE PERICARDIOCENTESIS:
Dr. Cooper performed a Pericardiocentesis from a subxiphoid approach without aspiration of blood on first attempt. The patient lost pulses during the second attempt.
AIRWAY REVISITED:
The ED team placed an ETT with direct laryngoscopy technique successfully on first pass attempt – NICE JOB DR. DEBAUN and DR. SAJADI!!!
BREATHING REVISITED:
Diminished breath sounds on left.
CIRCULATION REVISITED:
CPR started immediately. Massive transfusion protocol activated.
THE THORACOTOMY:
Dr. Cooper and the ED team initiated the resuscitative thoracotomy. After gaining access the the pleural cavity, the Trauma Team arrived and extended the incision while Dr. Cooper and the Trauma Team inserted and expanded the rib spreaders with a large volume blood evacuation suggesting Tension Hemothorax. The Trauma Team also expertly placed a right sided chest tube. The Trauma Team palpated a defect in the pericardium and right atrial wall from the penetrating injury. The Trauma team applied finger pressure to occlude the bleeding. They then inserted a Foley, which was inflated after entering the right atrium to tamponade the bleeding. Shortly thereafter, they delivered the heart through the pericardium. The patient regained cardiac function and CPR was stopped.
While Trauma was digitally occluding the cardiac defect, Dr. Cooper placed a subclavian CORDIS with assistance by Dr. Sajadi.
The patient received 4 units of blood and FFP in the ED.
THE OPERATING ROOM
The patient made it from the ED Trauma Bay to the OR under the care of Trauma Surgery and Anesthesia resulting in successful closure of the right atrial defect with a purse string repair.
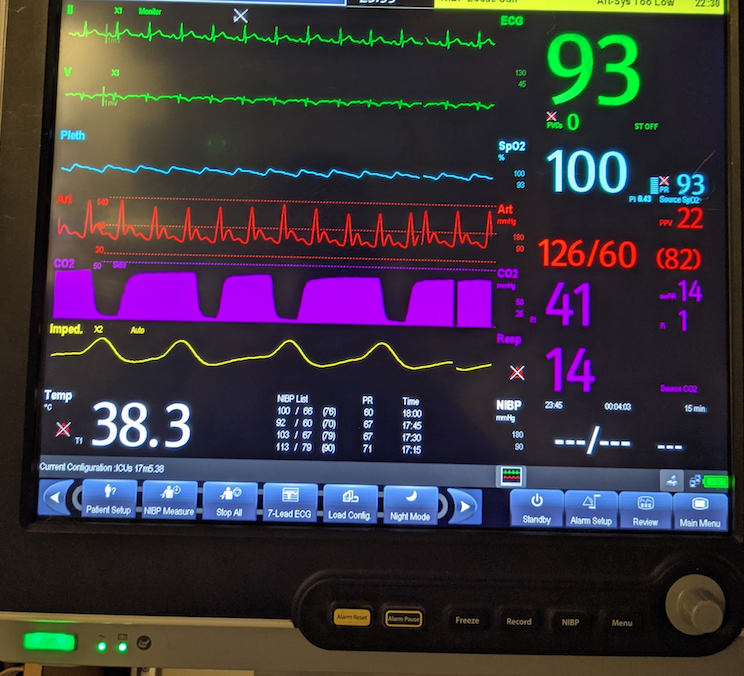
THE ICU:
Patient was then transferred to the ICU with fentanyl and propofol for sedation.
THE AFTERMATH:
Dr. Cooper reviewed the images and cleaned up his trusty trauma Ultrasound machine. Little did he know, 4 gunshot wound victims, 1 pediatric arrest and multiple strokes were ahead of him for the rest of his shift. Shortly after this incident, the team heard the new announcement made overhead: “Trauma Level 1, male patient, ETA 8 minutes”.