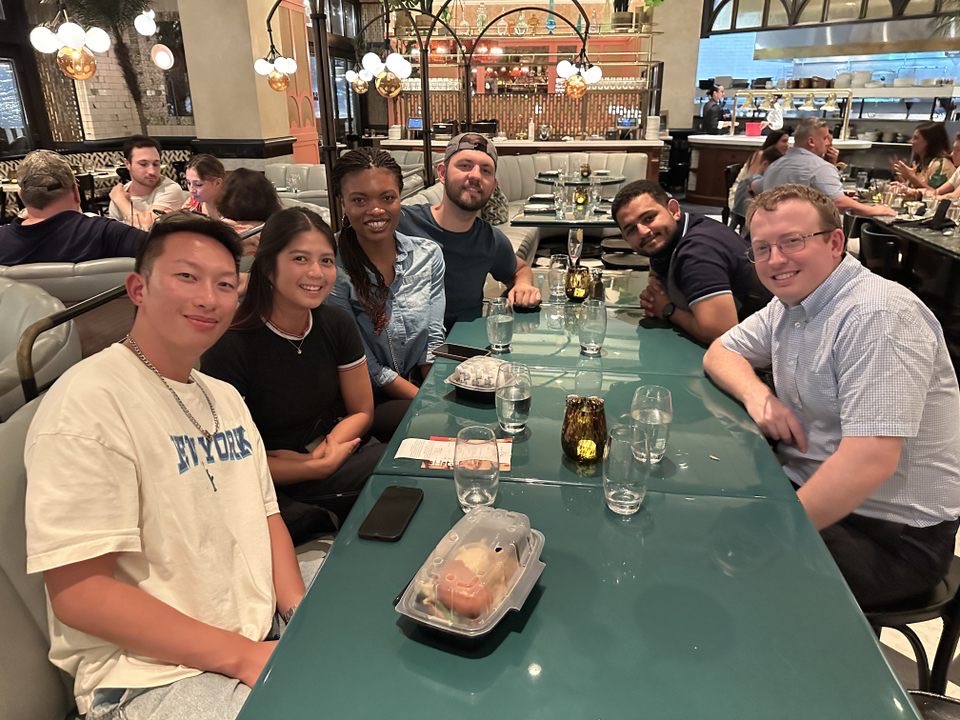
Resident resilience panel
July 8, 2021
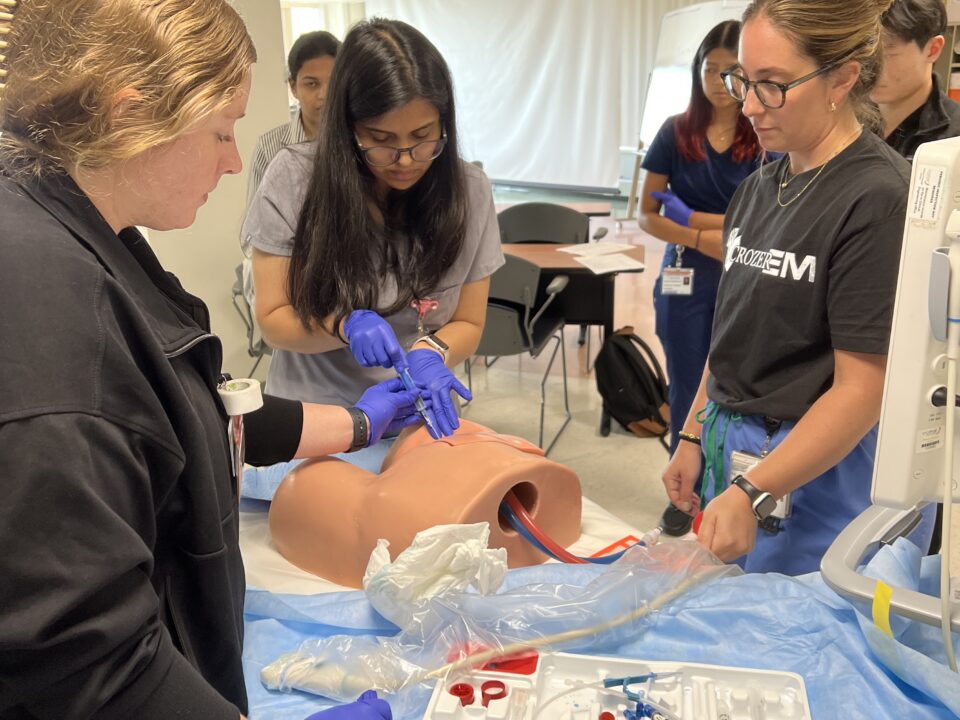
Cadaver Lab
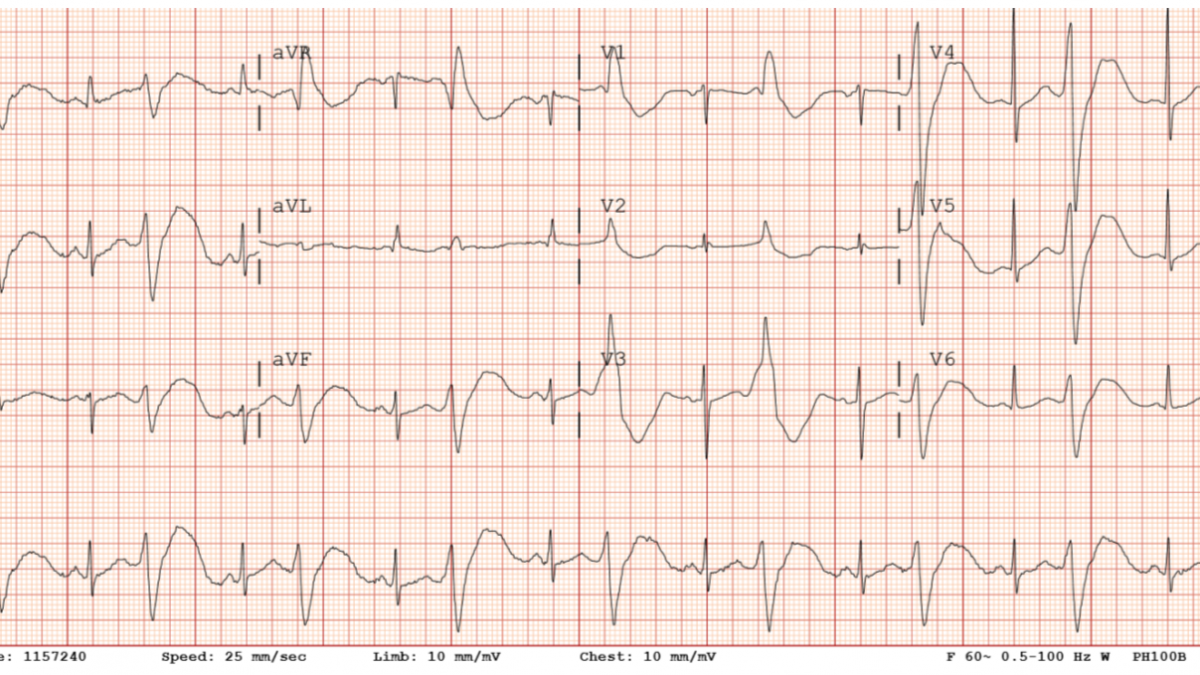
July 16, 2021HPI: 55-year-old female with a history of opioid abuse, anxiety, depression, AICD placed in 2006 for history of ventricular tachycardia and ventricular fibrillation, diabetes, and hypertension presents the emergency department stating that her AICD has fired multiple in the past day including about 30 minutes prior to arrival. She did experience palpitations before her AICD fired. The patient states that she did relapse and snort heroin yesterday before her AICD began shocking her. She denies other recent drug use, denies current symptoms, any other recent illnesses, or any other current complaints. She takes methadone 180 mg daily as well as Risperdal (unknown dose) at home.
ROS: Patient complaining that she is experiencing intermittent palpitations followed by firing of her AICD, all of these symptoms began after snorting heroin.
Physical Exam: Vitals stable, airway intact, heart was regular rate and rhythm during initial physical exam, patient was in no acute distress with a normal physical exam.
Results: Troponin 8 ng/L, Magnesium 1.8 mg/dl, Creatinine 1.1 mg/dl, WBC 11.1 10*3/uL, CXR showed mild interstitial thickening with no significant effusions, EKG showed normal sinus rhythm.
ED Course: Patient had multiple episodes of palpitations in the ED after which she was shocked by her AICD. Upon reviewing the monitor rhythm strip, patient appeared to be in wide complex ventricular tachycardia during the episodes. Previous to one of her AICD shocks, her rhythm appeared concerning for torsades de pointes. Patient received magnesium 2g IV, normal saline 1L IV, amiodarone 150 mg IV slow push, and was started on an amiodarone drip. Cardiology was consulted, agreed with the plan, and accepted the patient to inpatient cardiology service.
Hospital Course: EKGs showed lengthening QTCs over 550 in the hospital, so patient was switched from amiodarone to mexiletine. EP was consulted for AICD interrogation. Risperidone was held due to patient’s prolonged QTC. Psychiatry was consulted and recommended that if QTC was over 500 methadone should be held. The Patient spent three nights in the hospital and was discharged on her home methadone dose with improving QTC, as well of mexiletine 200 mg PO q8 hours.
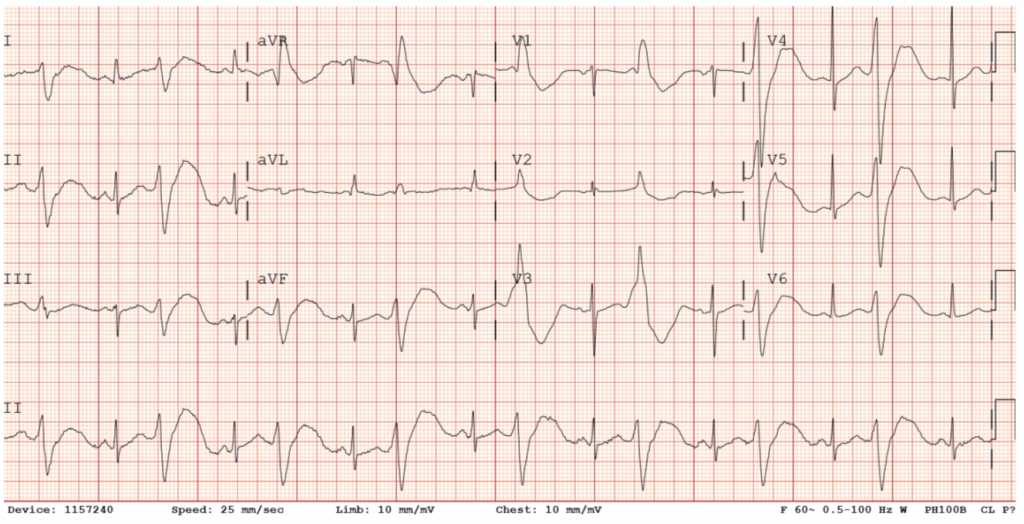
Initial EKG in the ED: Ventricular bigeminy with QTc of 551.
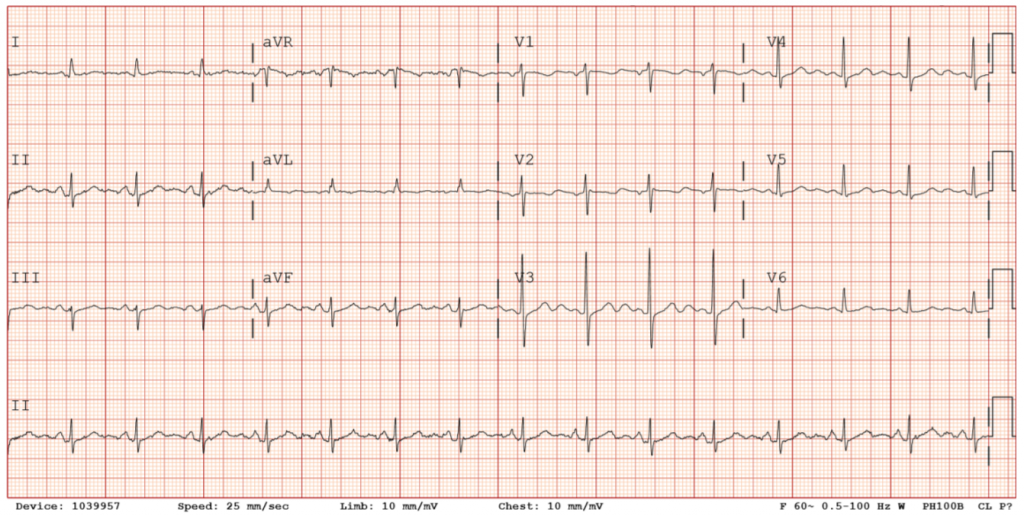
EKG on day of discharge: Normal sinus rhythm.
Summary: Patient with history of AICD for ventricular tachycardia was taking multiple QTC prolonging medications at home, as well as snorting heroin which can prolong QTC. These drugs combined likely caused the patient to have episodes of wide complex ventricular tachycardia / torsades de pointes, which prompted firing of her AICD. Magnesium and amiodarone were started for rhythm control, but mexiletine was eventually favored over amiodarone. Mexiletine is a class 1b antiarrhythmic medication that does not carry significant risk for QTC prolongation.